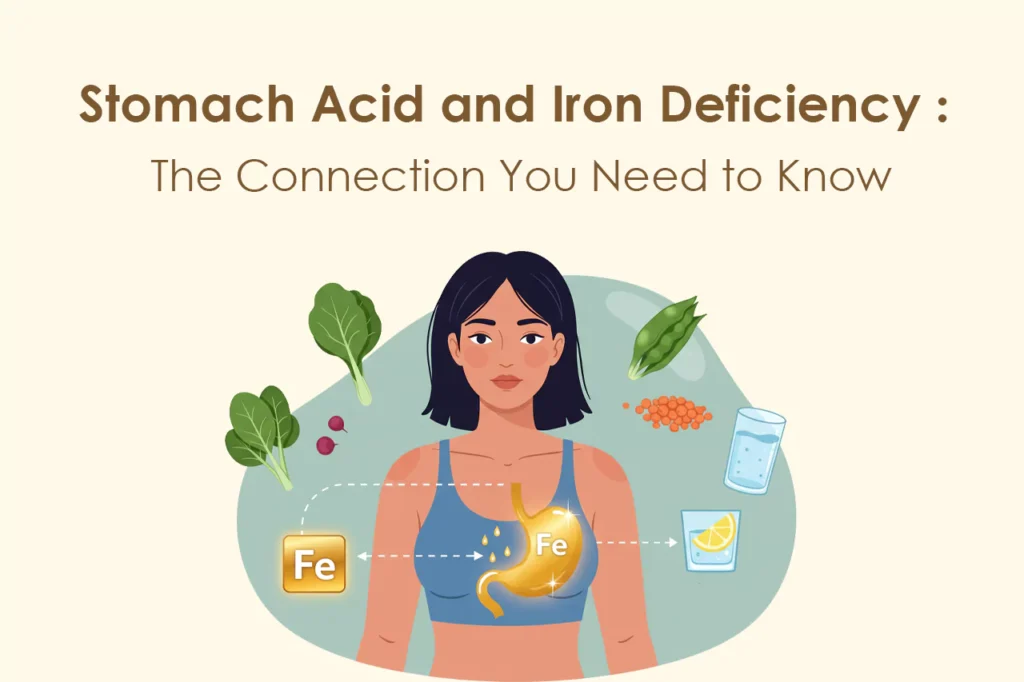
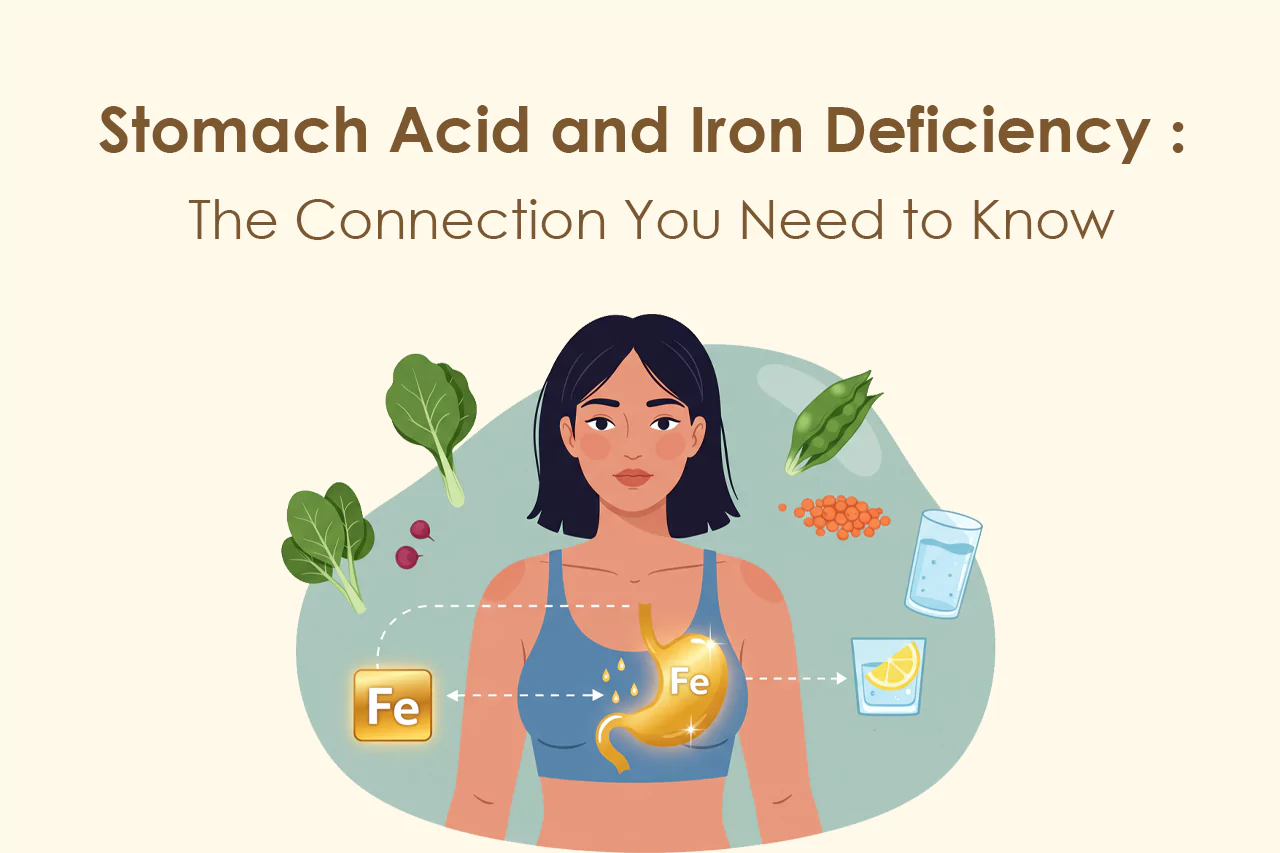
Stomach acid plays a central role in how the body processes food, absorbs nutrients, and defends against pathogens. Yet, it remains one of the most misunderstood and overlooked elements in conversations about health, especially when it comes to iron absorption and nutritional deficiencies. In this article, we’ll explore the connection between hydrochloric acid, iron, and overall well-being, offering evidence-based insight into a topic that deserves far more attention than it receives.
What Is Stomach Acid and Why Is It Important?
Hydrochloric acid (HCl), the primary component of stomach acid, is a powerful digestive fluid produced by the parietal cells in the stomach lining. Its primary role is to facilitate the breakdown of food, especially proteins, into smaller, more manageable components that can be further digested and absorbed in the small intestine.
Beyond digestion, stomach acid performs several other crucial functions:
- It sterilizes the stomach environment by killing harmful microbes that enter the body through food or water.
- It activates enzymes like pepsin, which are essential for protein digestion.
- It supports the absorption of key nutrients, particularly iron, calcium, magnesium, and vitamin B12.
When stomach acid levels are inadequate, a domino effect occurs: digestion slows, nutrients are lost, and the immune system is weakened.
The Role of Stomach Acid in Iron Absorption
Iron is an essential mineral responsible for producing hemoglobin, a protein in red blood cells that carries oxygen from the lungs to the rest of the body. There are two types of dietary iron: heme iron, found in animal products, and non-heme iron, found in plant-based foods.
Non-heme iron is particularly dependent on stomach acid for absorption. HCl helps convert ferric iron (Fe³⁺), which is poorly absorbed, into ferrous iron (Fe²⁺), a form that can pass through the intestinal wall and enter the bloodstream.
When stomach acid is low, this conversion is impaired. Even if someone consumes enough iron-rich foods, their body may not be able to absorb the mineral efficiently. Over time, this can result in iron deficiency or even iron-deficiency anemia, which is characterized by fatigue, pale skin, dizziness, and reduced immune resilience.
Vitamin B12, Intrinsic Factor, and Acid Levels
The role of stomach acid is not limited to iron. It is also essential for the absorption of vitamin B12, a nutrient critical to nerve function, red blood cell formation, and DNA synthesis.
For vitamin B12 to be absorbed, it must bind to a glycoprotein called intrinsic factor, also secreted by the stomach. If either stomach acid or intrinsic factor production is insufficient, vitamin B12 cannot be effectively absorbed in the small intestine.
Symptoms of B12 deficiency include numbness, memory issues, mood changes, fatigue, and in severe cases, neurological damage. This issue is particularly relevant for older adults and individuals with digestive disorders such as gastritis or autoimmune conditions like pernicious anemia.
What Causes Low Stomach Acid?
There are multiple factors that can contribute to hypochlorhydria or low stomach acid. The most common include:
- Aging: As we get older, the stomach’s ability to produce acid often decreases.
- Chronic stress: Long-term stress can downregulate digestive secretions, including HCl.
- Medications: Proton pump inhibitors (PPIs), antacids, and H2 blockers significantly reduce stomach acid production when taken long-term.
- Nutritional deficiencies: Zinc and vitamin B6 are needed for HCl production.
- H. pylori infection: This bacterial infection can damage the stomach lining and impair acid secretion.
Understanding the cause of low stomach acid is critical. In many cases, what appears to be “acid reflux” is actually the result of too little stomach acid, not too much. This leads to fermentation in the stomach, which produces gas and pushes acid into the esophagus.
How to Recognize Low Stomach Acid
The symptoms of low stomach acid are often confused with other digestive conditions, which makes it tricky to identify. Common signs include:
- Bloating, especially after eating
- Feeling full despite eating small amounts
- Frequent burping
- Undigested food in stool
- Iron or B12 deficiency
- Acid reflux or heartburn
- Gas or indigestion after protein-rich meals
Because these symptoms overlap with other gastrointestinal issues, testing is helpful for confirmation.
A Simple At-Home Test for Stomach Acid
One of the simplest ways to gauge stomach acid levels is the bicarbonate (baking soda) test. Although not diagnostic, it can offer preliminary insight.
- Mix 1/4 teaspoon of baking soda in 4 to 6 ounces of cold water.
- Drink it first thing in the morning on an empty stomach.
- Start timing immediately. If you belch within two to three minutes, your stomach likely has adequate acid.
- If belching takes longer or doesn’t happen at all, low stomach acid may be a factor.
This test should not be used as a replacement for clinical diagnostics, but it can serve as a starting point for further investigation.
Iron Deficiency: Causes, Symptoms, and Risk Factors
Iron deficiency remains one of the most common nutritional deficiencies worldwide. It is especially prevalent among women of childbearing age, vegetarians, frequent blood donors, and individuals with chronic digestive disorders.
Symptoms include:
- Persistent fatigue
- Pale or sallow skin
- Brittle nails and hair thinning
- Cold hands and feet
- Poor concentration
- Shortness of breath
- Headaches
- Restless leg syndrome
If left unaddressed, iron deficiency can progress into anemia, affecting daily functioning and overall health.
Supporting Stomach Acid and Digestive Health Naturally
There are practical steps you can take to support healthy stomach acid levels and optimize nutrient absorption:
- Eat Mindfully: Chew thoroughly and avoid eating in a rushed or stressed state. Digestion begins in the brain.
- Incorporate Bitter Foods: Arugula, dandelion greens, and radicchio stimulate the vagus nerve and promote stomach acid secretion.
- Limit Fluid During Meals: Drinking large amounts of water while eating can dilute stomach acid. Sip moderately.
- Supplement Cautiously: Betaine HCl, under practitioner supervision, may help raise stomach acid levels.
- Avoid Long-Term Antacid Use: Use antacids only when necessary and always under guidance.
- Include Fermented Foods: Sauerkraut, kefir, and kimchi support gut health and digestive enzyme activity.
Additionally, regularly consuming vitamin C-rich foods (such as citrus, kiwi, and bell peppers) alongside plant-based iron can enhance its absorption, especially when stomach acid is marginal.
Should You Be Concerned About Low Stomach Acid?
While many focus on consuming the right nutrients, few consider whether their body can actually absorb them. Stomach acid is the unsung hero in this equation. Without it, even the most nutrient-dense meals can leave the body undernourished.
If you’ve been dealing with unexplained fatigue, recurring infections, or stubborn iron deficiency, investigating your stomach acid levels may provide the missing piece of the puzzle. Talk with a qualified healthcare provider and consider nutritional testing when appropriate.